Antibiotic Choice Advisor
Recommended Antibiotic:
Antibiotic Comparison
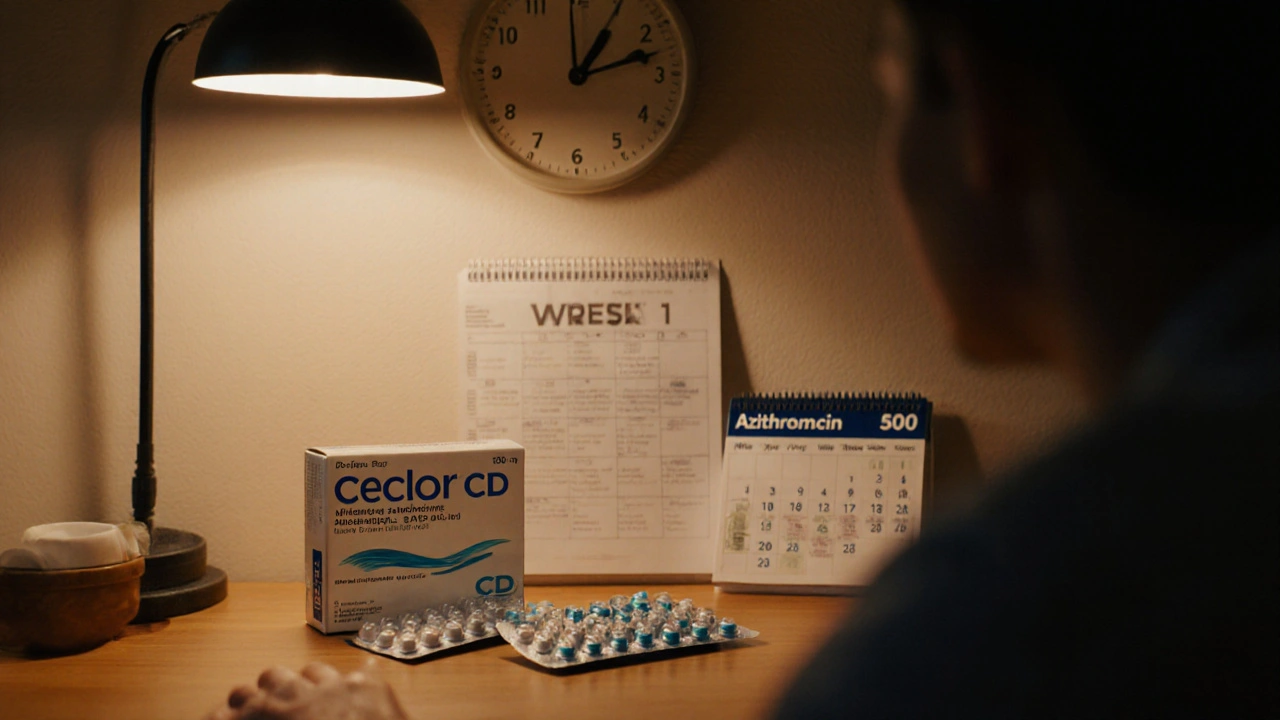
Ceclor CD
Second-gen cephalosporin
Good for sinusitis & otitis
Amoxicillin
Broad-spectrum penicillin
Cost-effective option
Azithromycin
Macrolide
Great for penicillin allergies
Key Takeaways
- Ceclor CD (cefaclor) is a second‑generation cephalosporin effective for many respiratory and ear infections, but it isn’t the only option.
- Amoxicillin offers a broader gram‑positive coverage and is usually cheaper.
- Cefdinir and cefuroxime providesimilar spectrums to Ceclorbut differ in dosing convenience and side‑effect profiles.
- Azithromycin, a macrolide, works well for patients allergic to beta‑lactams but has a narrower bacterial range.
- Choosing the right antibiotic depends on the infection type, bacterial resistance patterns, patient allergies, and dosing preferences.
What Is Ceclor CD?
Ceclor CD is the brand name for cefaclor, a second‑generation oral cephalosporin antibiotic. It was introduced in the early 1980s and quickly became a go‑to for middle‑ear infections, sinusitis, and uncomplicated pneumonia. Cefaclor works by inhibiting bacterial cell‑wall synthesis, a mechanism shared by all beta‑lactams.
Typical adult dosing is 250‑500mg every 6hours for 7‑10days, adjusted for kidney function. Because it’s a beta‑lactam, it’s generally safe for children over 6months, but it can trigger allergic reactions in people sensitive to penicillins.
How Ceclor CD Stacks Up Mechanistically
Cefaclor’s spectrum covers many gram‑positive cocci (like Streptococcus pneumoniae) and some gram‑negative rods (including Haemophilus influenzae). It’s less potent against Methicillin‑resistant Staphylococcus aureus (MRSA) and many beta‑lactamase‑producing strains.
Its pharmacokinetics are straightforward: good oral absorption (≈90%), moderate protein binding, and elimination primarily via the kidneys. This makes dose adjustment simple for patients with renal impairment.
Common Alternatives and When They Shine
Below are the most frequently prescribed competitors, each with its own sweet spot.
- Amoxicillin - a broad‑spectrum penicillin that’s cheaper and works well for ear infections, strep throat, and many community‑acquired pneumonias.
- Cefdinir - a third‑generation cephalosporin offering a slightly wider gram‑negative coverage, often chosen for patients who can’t tolerate amoxicillin.
- Cefuroxime - a second‑generation cephalosporin similar to cefaclor but with a longer half‑life, allowing twice‑daily dosing.
- Azithromycin - a macrolide used when beta‑lactam allergies exist; it’s convenient (once‑daily) but has a narrower bacterial range.
Side‑Effect Profiles Compared
All oral antibiotics share some common adverse events-nausea, diarrhea, and rash-but the incidence varies.
- Ceclor CD: mild GI upset in ~10% of users; rare C.difficile colitis.
- Amoxicillin: higher rates of diarrhea (≈12%) but lower rash risk for non‑allergic patients.
- Cefdinir: can cause dark stools and a higher chance of transient abdominal pain.
- Cefuroxime: similar GI profile to cefaclor but slightly more headache reports.
- Azithromycin: occasional QT‑prolongation concerns, especially with cardiac drugs.
Direct Comparison Table
| Antibiotic | Typical Adult Dose | Gram‑Positive Coverage | Gram‑Negative Coverage | Common Indications | Notable Side Effects |
|---|---|---|---|---|---|
| Cefaclor (Ceclor CD) | 250‑500mg Q6h | Good (S.pneumoniae, S.pyogenes) | Moderate (H.influenzae) | Sinusitis, Otitis media, Uncomplicated pneumonia | Diarrhea, Rash, Rare C.difficile |
| Amoxicillin | 500mg TID or 875mg BID | Excellent (Strep, S.pneumoniae) | Limited (H.influenzae) | Strep throat, Otitis media, Community‑acquired pneumonia | Diarrhea, Minor rash |
| Cefdinir | 300mg BID | Good | Broader (Enterobacter spp.) | Sinusitis, Pneumonia, Skin infections | Dark stools, Abdominal pain |
| Cefuroxime | 250‑500mg BID | Good | Moderate | Bronchitis, Otitis media, Uncomplicated pneumonia | Headache, Diarrhea |
| Azithromycin | 500mg QD × 3days | Fair (S.pneumoniae) | Limited (H.influenzae) | Chlamydia, Atypical pneumonia, Penicillin‑allergy cases | QT prolongation, Diarrhea |
Deciding Which Antibiotic Fits Your Situation
Consider these three decision points:
- Infection type: For classic bacterial sinusitis or middle‑ear infection, cefaclor or amoxicillin are first‑line. If the pathogen is suspected to be a resistant gram‑negative rod, cefdinir might be better.
- Allergy profile: Patients with penicillin allergies often receive cefaclor, cefuroxime, or azithromycin. However, cross‑reactivity between penicillins and cephalosporins is low (<5%), so a careful history can expand options.
- Convenience & cost: Amoxicillin’s BID regimen and low price make it popular for children. Cefuroxime’s BID dosing is easier than Ceclor’s Q6h schedule. Azithromycin’s three‑day course wins for compliance‑focused adults.
Talk to your prescriber about local resistance patterns. In many U.S. regions, Streptococcus pneumoniae remains largely susceptible to amoxicillin, making it a safe, inexpensive first choice.
Safety Tips and Drug Interactions
All of the antibiotics listed share key safety considerations:
- Renal function: Adjust doses of cefaclor, cefdinir, and cefuroxime when creatinine clearance <30ml/min.
- Probiotic use: Taking probiotics alongside any of these drugs can reduce diarrhea risk.
- Alcohol: No direct contraindication, but alcohol can worsen GI upset.
- Specific interactions:
- Cefaclor + oral anticoagulants may increase bleeding risk.
- Azithromycin + statins can raise muscle‑pain risk.
Never stop an antibiotic early, even if you feel better. Incomplete courses encourage resistance.
Frequently Asked Questions
Can I switch from Ceclor CD to amoxicillin if the infection isn’t improving?
Yes, but only after your doctor confirms the bacteria aren’t resistant to amoxicillin. A short culture or sensitivity test can guide the change.
Is cefaclor safe for children under 6 months?
Cefaclor is approved for infants older than 6 months. For younger babies, pediatricians usually prefer ampicillin or a narrower‑spectrum cephalosporin.
Why does cefaclor sometimes cause dark stools?
The drug contains iron‑based compounds that can color the stool. It’s harmless and resolves after the medication stops.
When should I consider azithromycin instead of a cephalosporin?
If you have a documented penicillin or cephalosporin allergy, or if you need a short, once‑daily regimen (e.g., travel‑related respiratory infection), azithromycin is a good alternative.
Can I take probiotics while on Ceclor CD?
Yes. Probiotics such as Lactobacillus rhamnosus can help maintain gut flora and may lessen diarrhea.


Comments (15)