When your eye doctor says you need an imaging test, it’s not just a routine check-it’s a window into the hidden layers of your retina, optic nerve, and blood vessels. Three key tools-OCT, fundus photography, and angiography-are now standard in diagnosing everything from diabetic eye disease to age-related macular degeneration. But what do they actually show? And why do doctors use all three instead of just one?
What OCT Shows That Other Tests Can’t
Optical Coherence Tomography (OCT) is like an ultrasound for your eye, but instead of sound waves, it uses light. It creates detailed cross-sections of your retina, showing each layer-down to micrometers. This isn’t just a picture; it’s a 3D map of your eye’s anatomy.Spectral-domain OCT (SD-OCT), the most common type today, can detect swelling in the macula before you even notice blurry vision. It spots tiny fluid pockets, thinning of retinal layers, or abnormal growths under the retina. For someone with diabetic retinopathy, OCT can tell if fluid is leaking into the macula-critical for deciding whether to start injections. In macular holes, it shows the exact size and depth. For glaucoma, it measures the thickness of the nerve fiber layer around the optic nerve.
newer swept-source OCT (SS-OCT) goes even deeper, imaging the choroid-the layer of blood vessels behind the retina-that older machines couldn’t clearly see. This matters because conditions like central serous chorioretinopathy or certain types of macular degeneration start in the choroid. SS-OCT also scans faster-up to 400,000 lines per second-making it better for patients who can’t hold still.
Unlike fundus photos, OCT doesn’t rely on clear vision or wide pupils. Even if your lens is cloudy from cataracts, OCT can still get a clear view of the retina. That’s why it’s often the first test ordered when something’s wrong.
Fundus Photography: The Big Picture
If OCT gives you a microscopic slice, fundus photography gives you the full landscape. These are color or infrared images of the back of your eye-retina, optic nerve, blood vessels, and macula-all in one frame.Doctors use fundus photos to track changes over time. A diabetic patient might get one every 6 to 12 months to see if new blood vessels are forming or if existing ones are leaking. A photo from 2023 can be compared to one from 2025 to see if macular degeneration is worsening. It’s also essential for documenting signs of hypertension, sickle cell disease, or even brain tumors that affect the optic nerve.
Modern cameras like the Zeiss FF 450+ capture high-resolution images in seconds. They can even take images without dilating your pupils, though dilation still gives the clearest view. The downside? If there’s any cloudiness in your eye-like a cataract or vitreous hemorrhage-the image can be blurry or blocked entirely. That’s why fundus photos are rarely used alone.
Fluorescein Angiography: Seeing Blood Flow in Real Time
Fluorescein angiography (FA) is the only test that shows how blood moves through your retina. A fluorescent dye is injected into your arm, and as it travels through the blood vessels in your eye, a special camera takes rapid-fire photos.This reveals leaks, blockages, and abnormal vessels that other tests miss. For example, in diabetic retinopathy, FA shows exactly where tiny blood vessels are leaking fluid into the retina. In wet age-related macular degeneration, it highlights the exact location of abnormal new blood vessels growing under the macula.
But FA has downsides. It’s invasive. You’ll feel a warm flush, and some people get nauseous. Rarely, there’s an allergic reaction. The whole process takes 10 to 30 minutes, and your skin and urine turn orange for hours. Plus, it can’t show the fine details of capillary networks-only the larger vessels.
Despite its drawbacks, FA remains the gold standard for detecting subtle leakage in diabetic macular edema. One study found FA was 100% sensitive in spotting leakage, while OCT only caught 79%. That 21% gap? It’s where patients could miss treatment if FA wasn’t done.
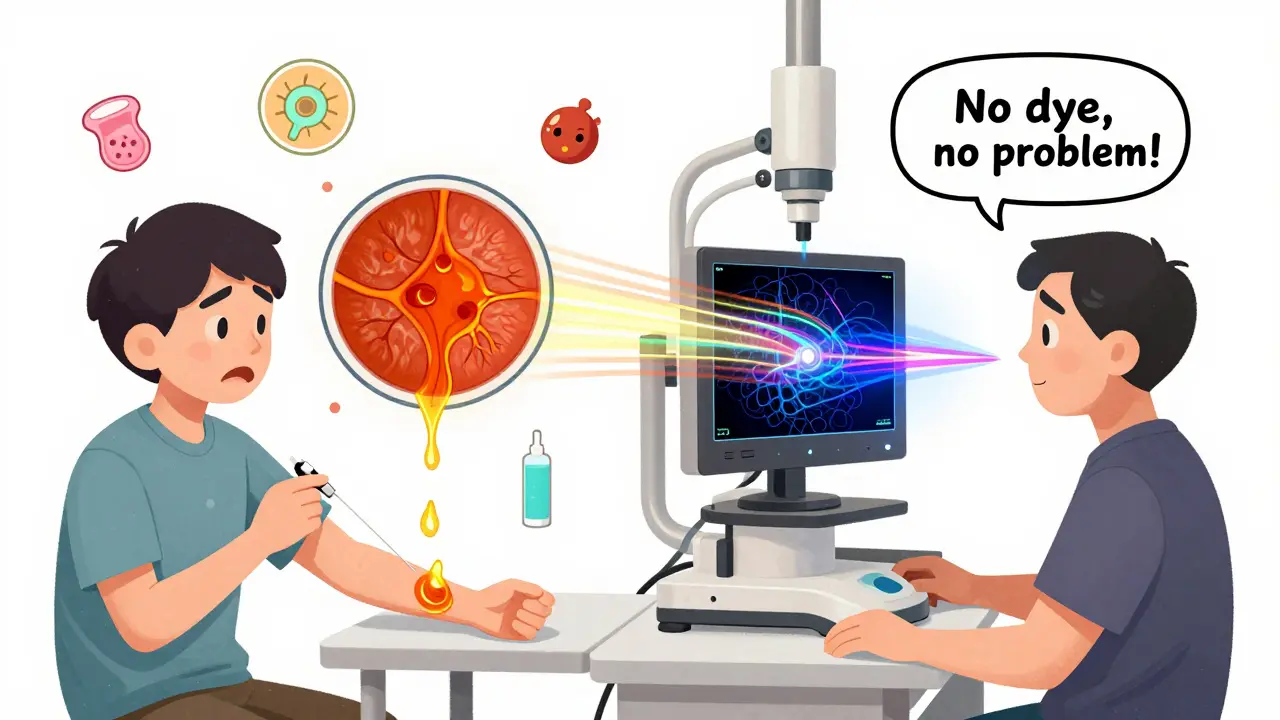
OCT Angiography: The Non-Invasive Revolution
OCT angiography (OCTA) is the newest player-and it’s changing everything. It gives you the same vascular detail as fluorescein angiography… without the dye.Using motion detection, OCTA tracks the movement of red blood cells to create 3D maps of retinal and choroidal blood flow. It can separate the capillary layers-superficial, middle, and deep-so doctors can see exactly where blood flow is reduced. In diabetic patients, it shows early signs of capillary dropout before vision loss occurs.
It’s faster than FA-seconds instead of minutes. No needles. No side effects. It’s especially helpful for children, elderly patients, or those with kidney problems who can’t handle dye.
But OCTA isn’t perfect. It can’t detect leakage. If a vessel is oozing fluid, OCTA won’t show it. It also struggles with motion-blinking or shifting your gaze can ruin the image. And while it’s great for detecting abnormal vessels, it can’t tell if they’re actively leaking or just present.
Studies show OCTA detects more microaneurysms and early neovascularization than FA in some cases. One study found it identified 57% more retinal capillary hemangiomas than older OCT systems. But it still can’t replace FA for certain conditions.
How Doctors Use Them Together
No single test tells the whole story. That’s why eye doctors use them in combination.For diabetic retinopathy:
- Fundus photo shows overall damage and new vessels.
- OCT confirms if fluid is in the macula.
- FA finds the exact leaking vessels.
- OCTA maps early capillary loss before it shows up on FA.
For age-related macular degeneration:
- OCT detects fluid or drusen.
- OCTA shows if new blood vessels are growing under the retina.
- FA confirms if those vessels are leaking (needed before treatment).
For rare diseases like Coats disease or punctate inner choroidopathy (PIC), OCT reveals hidden details: cholesterol crystals, fluid pockets under the retina, or tiny hyperreflective dots that match immune cells. FA might miss these entirely. OCTA then shows if the choroid’s blood flow is blocked.
What to Expect During Each Test
- OCT: You sit in front of a machine, rest your chin, look at a light. No contact. No drops. Takes 5-10 minutes.
- Fundus photo: Pupils may be dilated. You look at a bright flash. One or two quick snaps. Takes 5 minutes.
- Fluorescein angiography: A needle in your arm. You feel warmth, maybe nausea. Bright flashes every few seconds for 10-30 minutes. You’ll be orange for hours.
- OCTA: Same as OCT. No injection. No discomfort. Takes 3-5 minutes.
Most patients prefer OCTA or OCT because they’re quick and painless. FA is reserved for when the other tests aren’t enough.
Limitations and What’s Next
OCTA can’t show leakage. FA can’t show deep capillary layers. Fundus photos can’t show depth. OCT can’t show blood flow.That’s why no single test is enough. The future is integration. New AI tools are being trained to automatically detect diabetic retinopathy from OCT scans, or to flag areas of non-perfusion in OCTA images. Some clinics now use wide-field OCTA to scan the entire retina in one go-something FA could never do without multiple images.
As technology improves, OCTA may replace FA in many cases. But for now, FA still holds the edge in detecting active leakage. The best care combines all four tools: fundus photo for structure, OCT for anatomy, FA for leakage, and OCTA for detailed blood flow-all working together to protect your vision.

Comments (8)