Antibiotic Decision Tool
When you’re prescribed an antibiotic, you might not think twice about the name on the bottle-until you hear a friend say their doctor gave them something different. That’s when questions pop up: Is roxithromycin the best choice? What if it doesn’t work? Are there better options? The truth is, not all antibiotics are created equal, even when they’re in the same family. Roxithromycin is a macrolide antibiotic, used mainly for respiratory, skin, and soft tissue infections. But it’s not the only one out there. In fact, doctors often pick between roxithromycin, azithromycin, clarithromycin, or even amoxicillin based on your infection type, your history, and how your body reacts. This isn’t about which drug is ‘stronger.’ It’s about which one fits your situation best.
What is roxithromycin and how does it work?
Roxithromycin is a second-generation macrolide antibiotic, first approved in the 1980s. It works by stopping bacteria from making proteins they need to grow and multiply. Think of it like cutting off the supply line to a factory-the bacteria can’t build what they need to survive. It’s especially effective against Gram-positive bacteria like Streptococcus pneumoniae and Staphylococcus aureus, which cause things like strep throat, sinus infections, and mild skin infections. It also works against some atypical bacteria like Chlamydia pneumoniae and Mycoplasma, which often cause walking pneumonia.
Unlike older macrolides like erythromycin, roxithromycin is better absorbed by the body and lasts longer. That means you usually take it just once or twice a day, which makes it easier to stick to. It’s also less likely to cause stomach upset than erythromycin, though it can still happen. The standard adult dose is 150 mg once daily, or sometimes 300 mg every other day, depending on the infection. Treatment usually lasts 5 to 14 days.
Azithromycin: The most common alternative
If you’ve ever been prescribed an antibiotic for a sore throat or bronchitis, you’ve probably heard of azithromycin. Often sold as Zithromax or just called a ‘Z-pack,’ azithromycin is the most widely used alternative to roxithromycin. Like roxithromycin, it’s a macrolide, so it works the same way-but with some key differences.
Azithromycin has a longer half-life. That means it stays in your system longer, which is why you might only take it for 3 to 5 days instead of 7 to 14. A typical Z-pack is one 500 mg tablet on day one, then 250 mg daily for four more days. It’s convenient, which is why it’s so popular. But that convenience comes with trade-offs.
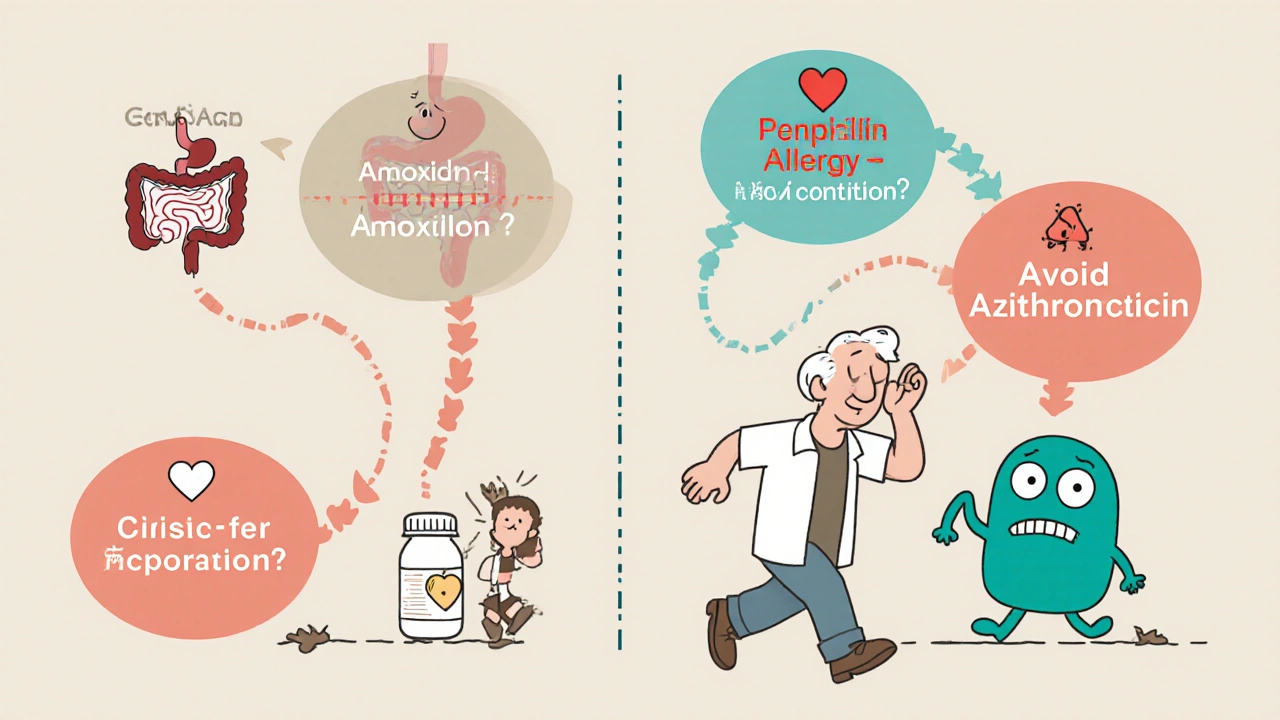
Studies show azithromycin is slightly more effective than roxithromycin for certain respiratory infections, especially those caused by Chlamydia pneumoniae. It’s also the go-to for sexually transmitted infections like chlamydia. However, azithromycin has a higher risk of causing heart rhythm problems in people with existing heart conditions. The FDA issued a warning about this in 2013. Roxithromycin doesn’t carry the same level of cardiac risk, making it a safer option for older adults or those with arrhythmias.
Clarithromycin: The close cousin
Clarithromycin, sold as Biaxin, is another macrolide that’s often compared to roxithromycin. It’s very similar in structure and function, but it’s more commonly used in the U.S. and Europe. It’s frequently prescribed for H. pylori infections (which cause stomach ulcers) when combined with other medications, something roxithromycin isn’t typically used for.
Both drugs are effective for sinusitis and bronchitis, but clarithromycin has slightly better penetration into lung tissue. That makes it a stronger choice for pneumonia. On the downside, clarithromycin interacts with more medications-especially statins, blood thinners, and some anti-seizure drugs. Roxithromycin has fewer drug interactions, which makes it a better fit if you’re already taking multiple prescriptions.
Another difference: clarithromycin can cause a metallic taste in the mouth, which some patients find unbearable. Roxithromycin doesn’t usually cause that. In clinical trials, patient adherence was higher with roxithromycin because side effects were milder overall.
Amoxicillin: The penicillin alternative
Not all antibiotics are macrolides. Amoxicillin, a penicillin-type drug, is often the first-line treatment for ear infections, strep throat, and uncomplicated pneumonia. It’s cheaper, widely available, and generally well-tolerated. But here’s the catch: if you’ve had a penicillin allergy-even a mild rash as a kid-amoxicillin is off the table.
Roxithromycin becomes a valuable alternative in those cases. It’s also preferred when the infection is caused by atypical bacteria that amoxicillin doesn’t cover well. For example, if your doctor suspects walking pneumonia (often caused by Mycoplasma), amoxicillin won’t help. Roxithromycin or azithromycin will.
But if your infection is caused by a typical strep bug, amoxicillin is still the gold standard. It kills bacteria faster and has fewer side effects than macrolides. The downside? Antibiotic resistance is growing. In some regions, up to 30% of strep throat cases no longer respond to amoxicillin. That’s where roxithromycin can step in as a second-line option.

When roxithromycin is the best choice
Roxithromycin isn’t always the first pick-but it’s often the smartest. Here’s when it shines:
- You have a mild to moderate respiratory infection and need something with fewer side effects than clarithromycin.
- You’re allergic to penicillin and need an oral antibiotic that’s still effective.
- You’re on other medications and want to avoid dangerous interactions.
- You’re over 65 and have a history of heart rhythm issues-azithromycin is risky here.
- Your infection is caused by atypical bacteria like Mycoplasma or Chlamydia pneumoniae.
It’s also a good option if you’ve tried amoxicillin and it didn’t work, or if you had bad stomach upset with erythromycin. Roxithromycin is gentler on the gut and still effective.
When roxithromycin isn’t the right fit
Not every infection responds to roxithromycin. It’s not effective against:
- Urinary tract infections (UTIs)-it doesn’t concentrate well in urine.
- Severe pneumonia requiring hospitalization-IV antibiotics are needed.
- Infections caused by resistant strains like MRSA (methicillin-resistant Staphylococcus aureus).
- Children under 4 months old-safety data is limited.
If your doctor suspects a UTI, they’ll likely reach for trimethoprim-sulfamethoxazole or nitrofurantoin. For severe pneumonia, ceftriaxone or levofloxacin might be better. Roxithromycin is for mild to moderate cases, mostly outpatient.
Side effects and safety: What to watch for
All antibiotics come with risks. Roxithromycin’s most common side effects are mild: nausea, diarrhea, stomach pain, and headache. These usually go away after a few days. Less than 2% of people stop taking it because of side effects, which is lower than clarithromycin (5%) and azithromycin (4%).
Rare but serious risks include liver problems (yellowing skin, dark urine) and allergic reactions (rash, swelling). If you notice these, stop taking it and call your doctor. Unlike azithromycin, roxithromycin doesn’t carry a black box warning for heart rhythm problems. That makes it safer for older patients or those with a history of QT prolongation.
It’s also not known to cause C. diff diarrhea as often as clindamycin or fluoroquinolones. That’s a plus if you’ve had that problem before.
Cost and availability
Roxithromycin is available as a generic, which keeps the cost low. In the U.S., a 10-day course can cost between $20 and $50 without insurance. In countries like Australia and the UK, it’s often cheaper than azithromycin. Azithromycin is more widely stocked in pharmacies, so if your local pharmacy doesn’t carry roxithromycin, you might need to order it or switch.
Insurance coverage varies. Some plans prefer azithromycin because it’s more commonly prescribed. If your insurance denies roxithromycin, your doctor can often write a letter explaining why it’s medically necessary-especially if you have allergies or drug interactions.
Real-world decision guide
So how do you decide? Here’s a simple flow:
- Is this a common cold or flu? → No antibiotic needed.
- Is it a sore throat with fever and swollen glands? → Test for strep. If positive and no penicillin allergy → amoxicillin. If allergic → roxithromycin or azithromycin.
- Is it a cough with low-grade fever and no green mucus? → Could be atypical pneumonia. → Roxithromycin or azithromycin.
- Are you on statins or blood thinners? → Avoid clarithromycin. Roxithromycin is safer.
- Are you over 65 with a heart condition? → Avoid azithromycin. Roxithromycin is preferred.
- Is this a skin infection like cellulitis? → Amoxicillin or cephalexin are better. Roxithromycin is not first-line.
The bottom line: roxithromycin isn’t the most famous antibiotic, but it’s one of the most practical. It’s effective, well-tolerated, and safer for many people than its competitors. It doesn’t replace all alternatives-but when the situation calls for a gentle, reliable, and interaction-friendly option, it’s often the best choice.
Is roxithromycin stronger than amoxicillin?
Neither is universally stronger. Amoxicillin kills common strep bacteria faster and is the first choice for strep throat and ear infections. Roxithromycin works better against atypical bacteria like Mycoplasma, which amoxicillin can’t touch. The right choice depends on the type of infection, not which drug is ‘stronger.’
Can I take roxithromycin if I’m allergic to penicillin?
Yes. Roxithromycin is a macrolide, not a penicillin, so it’s safe for people with penicillin allergies. It’s one of the most common alternatives prescribed in these cases. Always tell your doctor about any past allergic reactions, even if they were mild.
Does roxithromycin cause diarrhea like other antibiotics?
It can, but less often than many others. About 5-10% of users report mild diarrhea, compared to 15-20% with amoxicillin or clindamycin. It rarely causes severe C. diff infections, making it a safer option for people who’ve had antibiotic-related gut issues before.
How long does it take for roxithromycin to start working?
Most people notice improvement in symptoms within 2 to 3 days. For respiratory infections like sinusitis or bronchitis, fever and cough usually begin to ease by day 3. But you should still finish the full course-even if you feel better-to prevent the infection from coming back or becoming resistant.
Can I drink alcohol while taking roxithromycin?
There’s no dangerous interaction between roxithromycin and alcohol, unlike with metronidazole or some other antibiotics. But alcohol can worsen stomach upset or dehydration, which might make side effects feel worse. It’s best to avoid it while you’re sick and on antibiotics to give your body the best chance to recover.
Is roxithromycin safe for children?
Roxithromycin is approved for children over 4 months old, but only in specific cases like pertussis (whooping cough) or atypical pneumonia. It’s not typically used for ear infections or strep throat in kids-amoxicillin is preferred. Dosing is based on weight, and it should only be given under a doctor’s supervision.
Can roxithromycin treat a urinary tract infection (UTI)?
No. Roxithromycin doesn’t reach high enough concentrations in the urine to treat UTIs. Doctors use antibiotics like nitrofurantoin, trimethoprim-sulfamethoxazole, or fosfomycin instead. If you have a UTI and were given roxithromycin, ask your doctor why-it’s likely not the right choice.
What to do next
If you’ve been prescribed roxithromycin and are wondering if there’s a better option, don’t guess. Talk to your pharmacist or doctor. Bring a list of all your current medications. Ask: ‘Why this one? What happens if it doesn’t work? What are the alternatives?’ The goal isn’t to find the ‘best’ antibiotic-it’s to find the right one for you.
Antibiotic resistance is real. Using the wrong drug-or stopping early-makes it worse. Choosing the right one helps you get better faster and protects everyone else from harder-to-treat infections down the line.


Comments (8)